"The American Medical Association (AMA) is appalled by news from the Centers for Medicare and Medicaid Services (CMS) today that more than 50 percent of eligible professionals will face penalties under the Meaningful Use program in 2015, a number that is even worse than we anticipated.
Medical Billing Blog
Medicare Officials Announce Three Front-End Testing Weeks for ICD-10
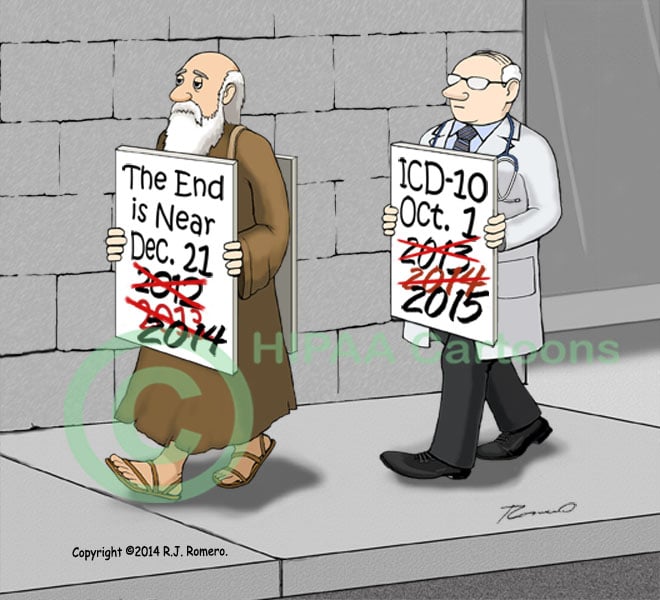
On August 22 the Centers for Medicare and Medicaid Services (CMS) announced that it would instruct Medicare Administrative Contractors (MACs) to hold three acknowledgement testing weeks for providers to prepare for the switch to ICD-10.
CMS Expects Some Bumps in Next Enrollment Period, but Says It Is Better Prepared
CMS Principal Deputy Administrator Andy Slavitt testified before the House Energy and Commerce Committee about a new report issued by the General Accounting Office (GAO) on CMS’ management of the healthcare.gov website.
CMS Seeks to Streamline Re-enrollment Process in Exchanges
The Department of Health and Human Services (HHS) announced a proposed rule to the Affordable Care Act (ACA) that would create more options for annual health plan eligibility redeterminations in the Exchanges, (both Federally-facilitated and state-based) as well as add more requirements for re-enrollment notices. If enacted, the rule would impact consumers who are re-enrolling in a Qualified Health Plan (QHP) during the 2015 open enrollment period (November 15, 2014 – February 15, 2015).
CMS Publishes Proposed 2015 Medicare Physician Fee Schedule
On Thursday, July 3rd, the Centers for Medicare and Medicaid Services released its proposed changes for the 2015 Medicare Physician Fee Schedule (PFS). The 600+ page proposed rule addresses changes to the physician fee schedule, and other Medicare Part B payment policies.
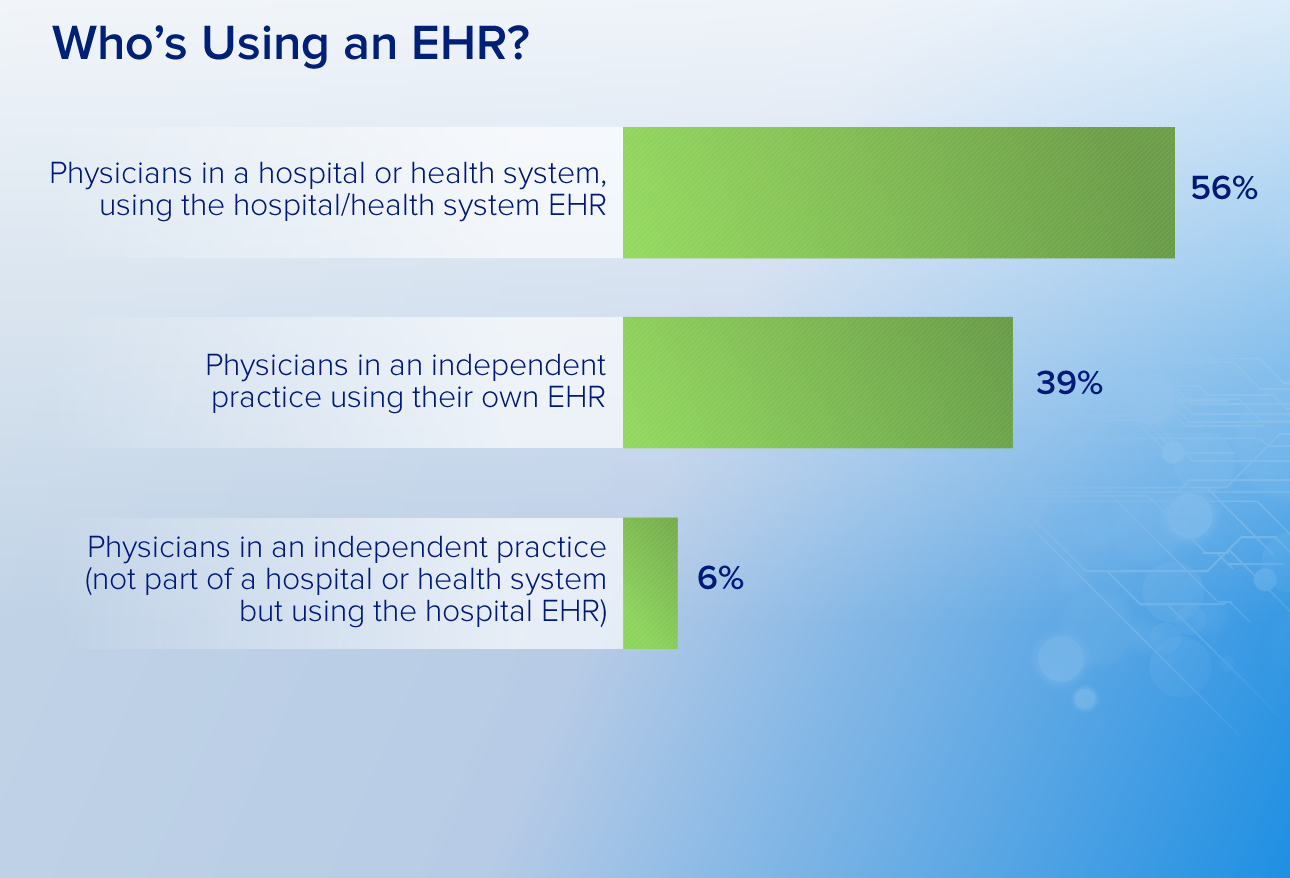
A recent survey of more than 18,500 physicians finds that 22 percent of them are opting out of or disregarding altogether the meaningful use electronic health records program.
New enrollments in Obamacare's Medicaid expansion and other healthcare programs for the poor have reached 6.7 million people since the launch of President Barack Obama's healthcare reforms last year, the administration said on Friday. CMS says about 26.4 million children were enrolled in CHIP or Medicaid overall, and 56 percent of all enrollees in the programs are children.
How Can Medicare Improve Improper Payment Prevention and Recoupment Efforts
Shortly before appearing before the House Oversight and Government Reform Committee, the Government Accountability Office (GAO) issued a report on Medicare mismanagement. The report summarizes existing program integrity procedures in the Medicare program and describes additional GAO program integrity recommendations that have yet to be implemented by CMS.
CMS Issues New Regulations for Medicare Part D Programs
This month the Centers for Medicare and Medicaid Services (CMS) issued final regulations for the Medicare Advantage and prescription drug benefit (Part D) programs. The proposed new requirements largely aim to improve the integrity and efficiency of Medicare Part C and Part D, the prescription drug program. CMS projects that the rule will save an estimated $1.615 billion over the next ten years 2015-2024.
How to Avoid 2016 PQRS Payment Adjustment in 2014
Individual eligible professionals (EPs) or those that are part of a group practice participating in PQRS must satisfactorily report data on quality measures during 2014 to avoid the 2016 payment adjustment. CMS has produced a document entitled 2016 PQRS Payment Adjustment that explains how to avoid the payment adjustment.