Q: What services can be provided by telehealth under the new emergency declaration?
A: CMS maintains a list of services that are normally furnished in-person that may be furnished via Medicare telehealth. This list is available here: https://www.cms.gov/Medicare/Medicare-GeneralInformation/Telehealth/Telehealth-Codes.
Q: Would physicians and other Qualified Providers be able to furnish Medicare telehealth services to beneficiaries in their homes?
A: Yes. The waiver temporarily eliminates the requirement that the originating site must be a physician’s office or other authorized healthcare facility and allows Medicare to pay for telehealth services when beneficiaries are in their homes or any setting of care.
Q: Who are the Qualified Providers who are permitted to furnish these telehealth services under the new law?
A: Qualified providers who are permitted to furnish Medicare telehealth services during the Public Health Emergency include physicians and certain non-physician practitioners such as nurse practitioners, physician assistants and certified nurse midwives. Other practitioners, such as certified nurse anesthetists, licensed clinical social workers, clinical psychologists, and registered dietitians or nutrition professionals may also furnish services within their scope of practice and consistent with Medicare benefit rules that apply to all services. This is not changed by the waiver.
Q: Will CMS enforce an established relationship requirement?
A: No. It is imperative during this public health emergency that patients avoid travel, when possible, to physicians’ offices, clinics, hospitals, or other health care facilities where they could risk their own or others’ exposure to further illness. Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act. To the extent the waiver (section 1135(g)(3)) requires that the patient have a prior established relationship with a particular practitioner, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
Q: Is any specialized equipment needed to furnish Medicare telehealth services under the new law?
A: Currently, CMS allows for use of telecommunications technology that have audio and video capabilities that are used for two-way, real-time interactive communication. For example, to the extent that many mobile computing devices have audio and video capabilities that may be used for two-way, real-time interactive communication they qualify as acceptable technology. The new waiver in Section 1135(b) of the Social Security Act explicitly allows the Secretary to authorize use of telephones that have audio and video capabilities for the furnishing of Medicare telehealth services during the COVID-19 PHE. In addition, effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency.
For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergencypreparedness/index.html
Q: How does a qualified provider bill for telehealth services?
A: Medicare telehealth services are generally billed as if the service had been furnished in-person. For Medicare telehealth services, the claim should reflect the designated Place of Service (POS) code 02-Telehealth, to indicate the billed service was furnished as a professional telehealth service from a distant site.
Q: How much does Medicare pay for telehealth services?
A: Medicare pays the same amount for telehealth services as it would if the service were furnished in person. For services that have different rates in the office versus the facility (the site of service payment differential), Medicare uses the facility payment rate when services are furnished via telehealth.
Q: Are there beneficiary out of pocket costs for telehealth services?
A: The use of telehealth does not change the out of pocket costs for beneficiaries with Original Medicare. Beneficiaries are generally liable for their deductible and coinsurance; however, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
Q: How long does the telehealth waiver last?
A: The telehealth waiver will be effective until the PHE declared by the Secretary of HHS on January 31, 2020 ends.
Q: Can hospitals, nursing homes, home health agencies or other healthcare facilities bill for telehealth services?
A: Billing for Medicare telehealth services is limited to professionals. (Like other professional services, Critical Access Hospitals can report their telehealth services under CAH Method II). If a beneficiary is in a health care facility (even if the facility is not in a rural area or not in a health professional shortage area) and receives a service via telehealth, the health care facility would only be eligible to bill for the originating site facility fee, which is reported under HCPCS code Q3014. But the professional services can be paid for.
Q: Can qualified providers let their patients know that Medicare covers telehealth?
A: Yes. Qualified providers should inform their patients that services are available via telehealth.
Q: Should on-site visits conducted via video or through a window in the clinic suite be reported as telehealth services?
A: Services should only be reported as telehealth services when the individual physician or professional providing the telehealth service is not at the same location as the beneficiary.
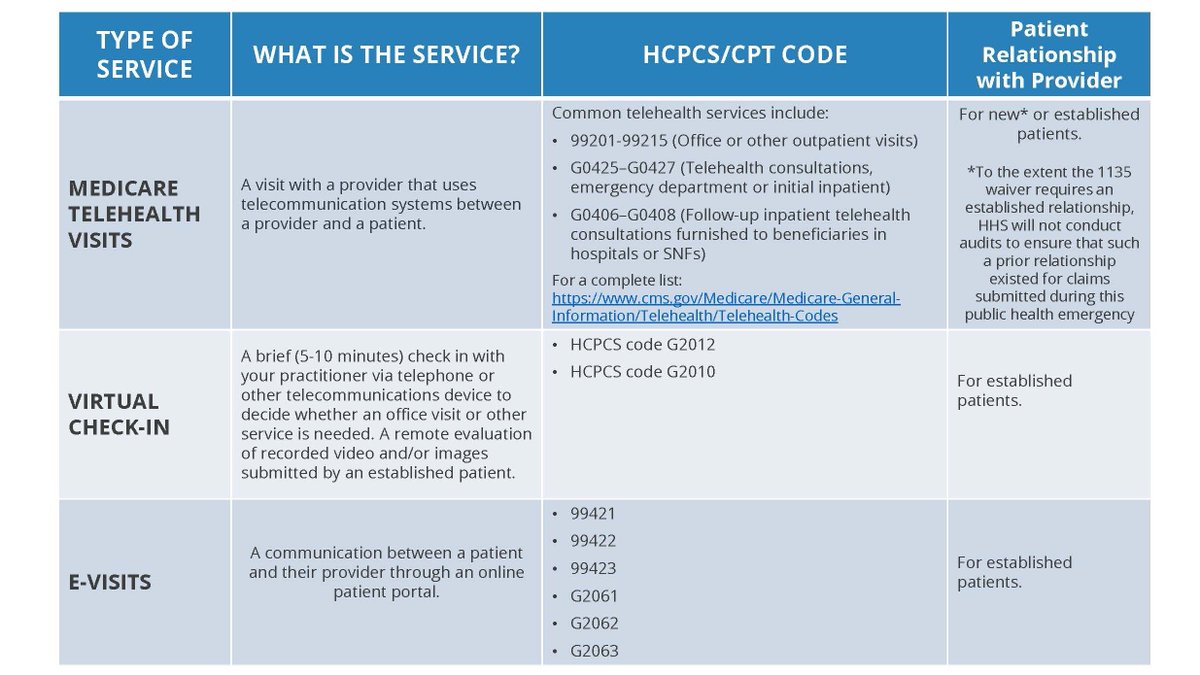
Q: How is this different from virtual check-ins and e-visits?
A: A virtual check-in pays professionals for brief (5-10 min) communications that mitigate the need for an in-person visit, whereas a visit furnished via Medicare telehealth is treated the same as an inperson visit, and can be billed using the code for that service, using place of service 02 to indicate the service was performed via telehealth. An e-visit is when a beneficiary communicates with their doctors through online patient portals.
Q: Are the telehealth services only limited to services related to patients with COVID-19?
A: No. The statutory provision broadens telehealth flexibility without regard to the diagnosis of the patient. This is a critical point given the importance of social distancing and other strategies recommended to reduce the risk of COVID-19 transmission, since it will prevent vulnerable beneficiaries from unnecessarily entering a health care facility when their needs can be met remotely. For example, a beneficiary could use this to visit with their doctor before receiving another prescription refill. However, Medicare telehealth services, like all Medicare services, must be reasonable and necessary under section 1862(a) of the Act.
Q: Will CMS require specific modifiers to be applied to the existing codes?
A: CMS is not requiring additional or different modifiers associated with telehealth services furnished under these waivers. However, consistent with current rules, there are three scenarios where modifiers are required on Medicare telehealth claims. In cases when a telehealth service is furnished via asynchronous (store and forward) technology as part of a federal telemedicine demonstration project in Alaska and Hawaii, the GQ modifier is required. When a telehealth service is billed under CAH Method II, the GT modifier is required. Finally, when telehealth service is furnished for purposes of diagnosis and treatment of an acute stroke, the G0 modifier is required.











