Dr. Shantanu Agrawal, MD, the Director of CMS’ Center for Program Integrity (CPI) stated that CPI is going to shift its focus to preventing fraud rather than chasing overpayments down after they have already been paid. In a speech to the American Bar Association’s Health Law Summit, Agrawal said that “preventative actions have a greater return on investment than the pay and chase model, in which the government seeks the return of overpayments it has already made”.
Medical Billing Blog
Hospitals Increasingly Outsourcing Coding Efforts
More hospitals are planning to outsource coding efforts in the coming year, according to a new survey published by Black Book Rankings.
Omnibus Rule Bridges Gap Between HIPAA & HITECH
On Jan. 25, 2013, the Department of Health and Human Services (HHS) published the “Omnibus Rule,” which is a final set of regulations that enforces various provisions of Health Information Technology for Economic and Clinical Health (HITECH) Act which in turn is designed to enhance the Health Insurance Portability and Accountability Act (HIPAA). In general, the new rules expand the obligations of physicians and other health care providers to protect patients’ protected health information (PHI), extend these obligations to who has access to PHI, and increase the penalties for violations.
There are basic areas providers will need to comply with:
CPR For Your ICD-10 Transition: Check, Prepare, Respond
The healthcare industry is changing rapidly and providers are facing many new challenges, with ICD-10, meaningful use, and fee schedule reductions being only a few. If you feel like there are just too many cats in the herd, there is one area where you can take control of the situation, and that is by re-evaluating the effectiveness and adaptability of your billing function. Whether you have an in-house billing staff, or an outsourced revenue cycle management team, it’s crucial to make an accurate assessment of the processes associated with your billing function to ensure that you are not part of the majority of practices expected to face serious cash flow problems when ICD-10 goes into effect next October.
HIPAA and HITECH Evolution Responds To Technological Advances
The HITECH Act (Health Information Technology for Economic and Clinical Health) was passed in February 2009 as part of the American Recovery and Reinvestment Act, it expanded the obligations of covered entities and business associates to protect the confidentiality and security of Protected Health Information (PHI). Passage of the HITECH Act was timely because its main purpose was to address voids inherent in HIPAA due to the development of new technologies that did not exist at the time HIPAA was originally implemented.
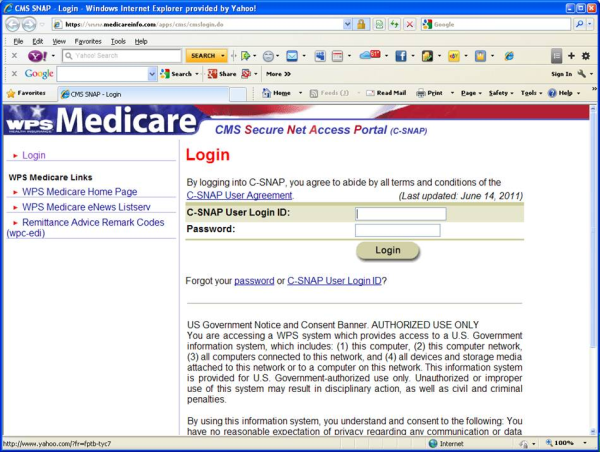
Revised Warnings For Docs Using Cloned Notes
As a follow up to my recent post “Avoiding Payment Denials for Cloned Notes,” the Centers for Medicare & Medicaid Services (CMS) has issued new instructions to Medicare Administrative Contractors (MAC’s), Recovery Audit Contractors (RAC’s), and Zone Program Integrity Contractors (ZPIC’s) to look for claims generated from Electronic Health Records (EHR’s) that do not contain adequate information.
Medicare Administrative Contractors (MACs) warn that individualized patient notes are required for each patient visit, and that use of “cloned notes” may cause a provider to overlook new information, resulting in treatment, safety, and quality issues.
ICD-10 May Defeat In House Billing Efforts
Providers should start preparing now for the implementation of ICD-10, which is scheduled to begin October 1, 2014. Basically let’s talk about getting your practice's infrastructure in order.
High-level E&M Codes Increase Risk of RAC Audit
Recovery Audit Contractors (RAC’s) are now reviewing high level evaluation and management (E&M) codes used in billing office visits in private practice. E&M services are based on the providers understanding of the patient’s medical history, review of patient’s medications, a physical examination, and of course a medical decision. According to Charles Fidel of AMedNews.com, Medicare paid $33.5 billion for E&M services in 2010. Of the 442,000 physicians that billed for E&M services, only 1,669 providers consistently billed high-level E&M codes such as 99215. A claim for a low-level visit by an established patient only paid about $20 in 2010, while a high-level new patient paid around $190.
Check Patient Eligibility For Wellness Visits To Ensure Reimbursement
Following on the heels of our recent article, “Billing and Coding for the Medicare Annual Wellness Visits,” we got this comment from a reader: