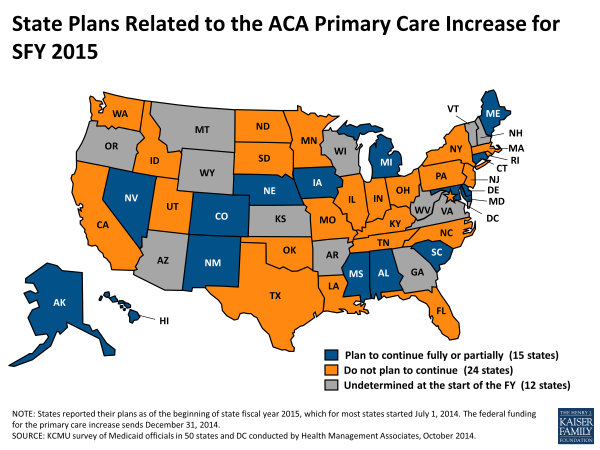
As part of the Patient Protection and Affordable Care Act (ACA) Medicaid payments for “primary care” services were temporarily increased to Medicare payment levels. Under this incentive program, the federal government fully funded the difference between what Medicaid would have paid physicians for the delivery of primary care services and what the comparable Medicare payment would be for that same service. The federal government’s enhanced contribution expired on December 31, 2014.
Medical Billing Blog
Medicaid Primary Care Incentive Payments Expire
Improper Payments: Government Wide Estimates and Reduction Strategies
Six States and D.C. Extend Medicaid Pay Raise for Primary Care Doctors
Six states and the District of Columbia. will use their own money in 2015 to sustain the federal Medicaid pay raise to primary care doctors. The pay raise stems from a provision of the Affordable Care Act (ACA) that expands Medicaid fees for primary care to the same amount paid under Medicare. The states are Maryland, Colorado, New Mexico, Iowa, Alabama, and Mississippi. Interestingly, Mississippi and Alabama did not participate in the Medicaid expansion under the ACA.
New enrollments in Obamacare's Medicaid expansion and other healthcare programs for the poor have reached 6.7 million people since the launch of President Barack Obama's healthcare reforms last year, the administration said on Friday. CMS says about 26.4 million children were enrolled in CHIP or Medicaid overall, and 56 percent of all enrollees in the programs are children.
Medicaid Enrollment Shows Continued Growth in April
The U.S. Department of Health and Human Services (HHS) released its Medicaid Enrollment Report for April, 2014. As of the end of April, 6 million more individuals were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP) as compared to the period before the initial open enrollment under the Affordable Care Act started in October, 2013. That includes 1.1 million additional people enrolled in April as compared to March in the 48 states that reported data for both April and March.
CBO Projects Health Law Subsidies Will Cost Less than Expected
Health-insurance premiums for plans sold in the Affordable Care Act's exchanges will be lower than previously expected for the next few years, according to a report by the Congressional Budget Office released Monday. The Congressional Budget Office predicts that health insurance subsidies under the Affordable Care Act will total a little more than $1 trillion over the next 10 years, instead of almost $1.2 trillion initially estimated. CBO said the 8 percent cut results largely from tighter cost controls by insurance companies offering plans on health care exchanges. Generally speaking, the plans offered on the exchanges pay health care providers less and have tighter management of patients’ treatment options, and that means lower premiums and taxpayer subsidies.
Medicaid Expansion in Michigan Starts April 1st
The state of Michigan has officially rolled out its Medicaid expansion program. Governor Rick Snyder, a Republican, fought his GOP-controlled legislature last summer to push through the expansion. But lawmakers refused to let it take effect earlier than April 1. Eligibility for this year is expected to be around 320,000 people. Further expansion is expected to cover about 470,000 residents through increasing the income limit for eligibility. Some elements of Michigan's Medicaid expansion program will require CMS approval. Currently, in order to qualify, adults must between the ages of 19 and 64 who are not currently eligible for Medicaid or Medicare, and are making less than 133 percent of the federal poverty line. The current FPL is about $16,000 for a single person and $33,000 for a family of four. The state plan notably includes a provision requiring enrollees after four years to seek exchange coverage or share some of the costs to remain in the Medicaid program. Interest in the Michigan program looks strong early on. By 4 p.m. Tuesday, the state reportedly received almost 12,000 applications for coverage.
Twenty-five people were charged Thursday with obtaining at least $75 million in fraudulent Medicaid payments from the District of Columbia government, a series of cases that federal prosecutors said added up to the largest health-care fraud in the city’s history. U.S. Attorney Ronald C. Machen Jr. said agents fanned out across the D.C. region to make arrests and seize six luxury vehicles and 49 bank accounts, capping off a multiyear investigation. Prosecutors said personal health care in private homes is a thriving front in Medicaid fraud, a category of Medicaid claims that has grown dramatically in the city over the past 8 years, and said there have been similar cases out of Miami and Detroit. The uptick in billings for home care — from $40 million in 2006 to $280 million last year — was part of what tipped off authorities to illegal activity, U.S. Attorney Ronald Machen said. Prosecutors say many of the defendants persuaded patients to fake illness or injury so they could bill Medicaid for home care they didn’t receive. Some of those patients received kickbacks, authorities said, although no patients have been charged. Those charged include the owners of home-care firms and nurse staffing agencies, home-care aides and recruiters who signed up patients.


.gif)