Government spending on “compounded” drugs that are handmade by retail pharmacists has skyrocketed, drawing the attention of federal investigators who are raising fraud and overbilling concerns.
Medical Billing Blog
Fraud Concerns Emerge As Compounding Drug Sales Skyrocket
United's Departure From Marketplaces Could Impact Consumers' Costs, Access
UnitedHealthcare’s decision to quit insurance exchanges in about 30 states next year has patient advocates concerned that fewer options could force consumers to pay more for coverage and have a smaller choice of network providers.
MedPAC approves a Number of New Recommendations
The Medicare Payment Advisory Commission (MedPAC) is a nonpartisan legislative branch agency that provides the U.S. Congress with analysis and policy advice on all aspects of the Medicare program (cost, reimbursement, access, quality, etc.). MedPAC issues two annual reports to Congress, one in March and another in June. These reports contain the policy recommendations of the Commission.
With the approaching deadline for enactment of an SGR fix, the similarities to last year’s situation has not been lost on many people when it comes to the possibility that Congress will once again step in to delay the October 1, 2015 effective date for adoption and use of ICD-10 codes.
SGR is the Top Healthcare Issue for Congress in 2015
According to several Congressional leaders, preventing a 21% cut in Medicare Physician Fee Schedule payments in 2015 under the flawed Sustainable Growth Rate (SGR) formula remains the top healthcare priority for Congress this year. The latest SGR cut is scheduled to take effect when the current short-term patch expires at midnight on March 31st.
Obamacare is about to collide with the U.S. tax-filing season, adding frustration for millions of taxpayers trying to figure out how to comply and how much they will owe the government.
Supreme Court to Hear King v. Burwell Arguments on March 4th
The US Supreme Court has scheduled oral arguments for King v. Burwell for March 4, 2015. This case will determine whether people purchasing health insurance via the Federal Health Exchange (healthcare.gov) are eligible to receive Federal subsidies towards their monthly premiums.
Meaningful Use Program Continues to Disappoint
As 2014 came to a close, the Meaningful Use program continued to fall short of its intended goals. Although more than 500,000 providers have registered for the Meaningful Use program, only 4% of professionals and 35% of hospitals have attested to Stage 2 of the program. These disappointing numbers come despite the fact that CMS watered down some of the requirements and moved the deadline back from November 30th to December 31st. Many providers are calling for the CMS to reduce its 365 day reporting requirement to 90 days but CMS remains steadfast behind the 365 day requirement.
Dr. Shantanu Agrawal, MD, the Director of CMS’ Center for Program Integrity (CPI) stated that CPI is going to shift its focus to preventing fraud rather than chasing overpayments down after they have already been paid. In a speech to the American Bar Association’s Health Law Summit, Agrawal said that “preventative actions have a greater return on investment than the pay and chase model, in which the government seeks the return of overpayments it has already made”.
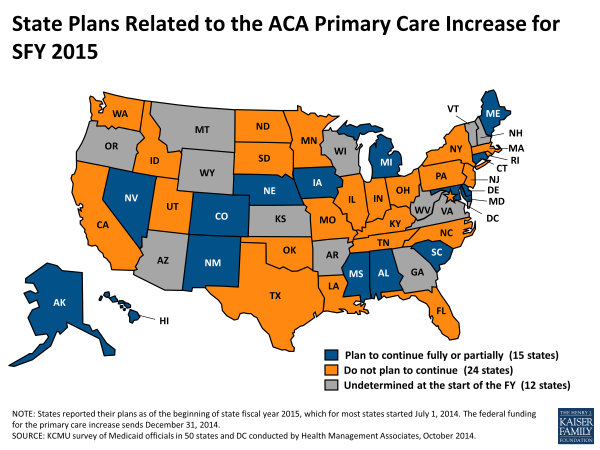
Medicaid Primary Care Incentive Payments Expire
As part of the Patient Protection and Affordable Care Act (ACA) Medicaid payments for “primary care” services were temporarily increased to Medicare payment levels. Under this incentive program, the federal government fully funded the difference between what Medicaid would have paid physicians for the delivery of primary care services and what the comparable Medicare payment would be for that same service. The federal government’s enhanced contribution expired on December 31, 2014.