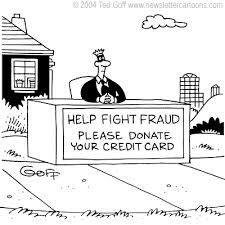
Government spending on “compounded” drugs that are handmade by retail pharmacists has skyrocketed, drawing the attention of federal investigators who are raising fraud and overbilling concerns.
Medical Billing Blog
Fraud Concerns Emerge As Compounding Drug Sales Skyrocket
Dr. Shantanu Agrawal, MD, the Director of CMS’ Center for Program Integrity (CPI) stated that CPI is going to shift its focus to preventing fraud rather than chasing overpayments down after they have already been paid. In a speech to the American Bar Association’s Health Law Summit, Agrawal said that “preventative actions have a greater return on investment than the pay and chase model, in which the government seeks the return of overpayments it has already made”.
Improper Payments: Government Wide Estimates and Reduction Strategies
Special Fraud Alert: Laboratory Payments to Referring Physicians
The HHS OIG released a Special Fraud Alert addressing compensation paid by laboratories to referring physicians and physician group practices (collectively, physicians) for blood specimen collection, processing and packaging, and for submitting patient data to a registry or database.
How Can Medicare Improve Improper Payment Prevention and Recoupment Efforts
Shortly before appearing before the House Oversight and Government Reform Committee, the Government Accountability Office (GAO) issued a report on Medicare mismanagement. The report summarizes existing program integrity procedures in the Medicare program and describes additional GAO program integrity recommendations that have yet to be implemented by CMS.
CMS: Isn't Cost-Effective to Review Billings of Doctors
Medicare, the national federal insurance program for Americans aged 65 and older, issued $6.7 billion in 2010 for health care visits that were improperly coded according to the report from the inspector general of the Department of Health and Human Services. But in its reply to the findings, the Centers for Medicare and Medicaid Services, which runs Medicare, said it doesn't plan to review the billings of doctors who almost always charge for the most expensive visits because it isn't cost-effective to do so.
Health Subcommittee Holds Hearing to Improve Medicare Oversight
On April 30th, the House Committee on Ways and Means Subcommittee on Health held a hearing to solicit input from the HHS Inspector General’s office (OIG), CMS and the Government Accountability Office (GAO) on ways to improve Medicare oversight and reduce waste, fraud and abuse. Gloria Jarmon, Deputy Inspector General for Audit Services, Office of Inspector General, testified on behalf of HHS; Shantanu Agrawal, M.D., Deputy Administrator and Director, Center for Program Integrity, testified on behalf of CMS; and Kathy King, Director, Health Care testified on behalf of GAO.
Proposed Fiscal Budget 2015 - A Healthcare Analysis
On Tuesday, March 4, the Office of Management and Budget (OMB) released the President’s budget for Fiscal Year (FY) 2015. This budget is not a binding document and will likely result in no real action. The President’s budget is considered an indication of the President’s priorities for the upcoming fiscal year. It is important to understand the budget because certain provisions of it may be included in future proposals and legislation.
Twenty-five people were charged Thursday with obtaining at least $75 million in fraudulent Medicaid payments from the District of Columbia government, a series of cases that federal prosecutors said added up to the largest health-care fraud in the city’s history. U.S. Attorney Ronald C. Machen Jr. said agents fanned out across the D.C. region to make arrests and seize six luxury vehicles and 49 bank accounts, capping off a multiyear investigation. Prosecutors said personal health care in private homes is a thriving front in Medicaid fraud, a category of Medicaid claims that has grown dramatically in the city over the past 8 years, and said there have been similar cases out of Miami and Detroit. The uptick in billings for home care — from $40 million in 2006 to $280 million last year — was part of what tipped off authorities to illegal activity, U.S. Attorney Ronald Machen said. Prosecutors say many of the defendants persuaded patients to fake illness or injury so they could bill Medicaid for home care they didn’t receive. Some of those patients received kickbacks, authorities said, although no patients have been charged. Those charged include the owners of home-care firms and nurse staffing agencies, home-care aides and recruiters who signed up patients.
MBR Explains: Quality Improvements - Key Features of the Affordable Care Act by Year -- 2010
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2010 that sought to improve quality and lower cost of healthcare. As previously mentioned, the Patient Protection and Affordable Care Act was signed by President Obama on March 23, 2010. The law aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key quality improvement provisions that took effect in 2010.