The healthcare industry is changing rapidly and providers are facing many new challenges, with ICD-10, meaningful use, and fee schedule reductions being only a few. If you feel like there are just too many cats in the herd, there is one area where you can take control of the situation, and that is by re-evaluating the effectiveness and adaptability of your billing function. Whether you have an in-house billing staff, or an outsourced revenue cycle management team, it’s crucial to make an accurate assessment of the processes associated with your billing function to ensure that you are not part of the majority of practices expected to face serious cash flow problems when ICD-10 goes into effect next October.
Medical Billing Blog
CPR For Your ICD-10 Transition: Check, Prepare, Respond
A recent survey conducted by the Workgroup for Electronic Data Interchange (WEDI) regarding the preparations for transitioning to ICD-10 being conducted by healthcare providers shows that nearly half of the survey group either have not started preparing for ICD-10 or do not know when they expect to start their testing.
Managing a successful medical practice involves more than just practicing medicine. You must also view it as a successful business, and put into place sound business practices, as well. Many providers are seeing their revenues decline as payers are reducing fee schedules, so it’s more important than ever to collect every dollar that you’re entitled to, and to manage how you budget that revenue to keep your practice running in the black.
HIPAA and HITECH Evolution Responds To Technological Advances
The HITECH Act (Health Information Technology for Economic and Clinical Health) was passed in February 2009 as part of the American Recovery and Reinvestment Act, it expanded the obligations of covered entities and business associates to protect the confidentiality and security of Protected Health Information (PHI). Passage of the HITECH Act was timely because its main purpose was to address voids inherent in HIPAA due to the development of new technologies that did not exist at the time HIPAA was originally implemented.
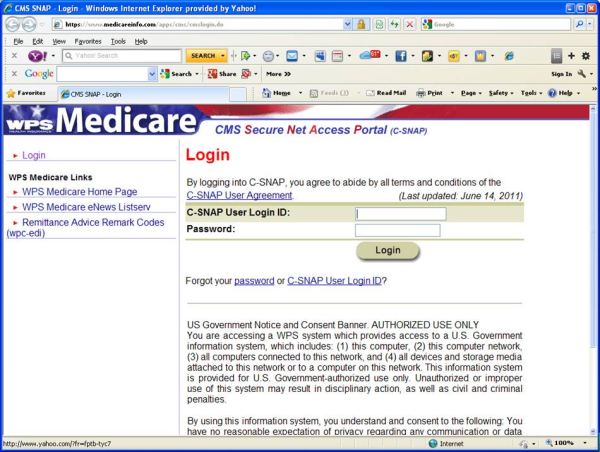
Revised Warnings For Docs Using Cloned Notes
As a follow up to my recent post “Avoiding Payment Denials for Cloned Notes,” the Centers for Medicare & Medicaid Services (CMS) has issued new instructions to Medicare Administrative Contractors (MAC’s), Recovery Audit Contractors (RAC’s), and Zone Program Integrity Contractors (ZPIC’s) to look for claims generated from Electronic Health Records (EHR’s) that do not contain adequate information.
Use Better Collection Techniques To Increase Patient Payments
It is said that “a bird in the hand is worth two in the bush,” and that is especially true when you’re talking about collecting payments from patients at the time of service. According to the AMA, the average cost to physicians for collecting monies owed and processing claims is 10 – 14 percent of gross revenue, butthere are ways to be more efficient, reduce these costs, and collect payments faster. The AMA website offers a Point-of-Care Pricing Toolkit to help you collect payment from patients before they walk out the door.
ICD-10 May Defeat In House Billing Efforts
Providers should start preparing now for the implementation of ICD-10, which is scheduled to begin October 1, 2014. Basically let’s talk about getting your practice's infrastructure in order.
The Centers for Medicare & Medicaid Services (CMS) on November 1, 2012 issued its 1,362-page final rule of fee schedules for 57 physician and other specialty provider groups for calendar year 2013.
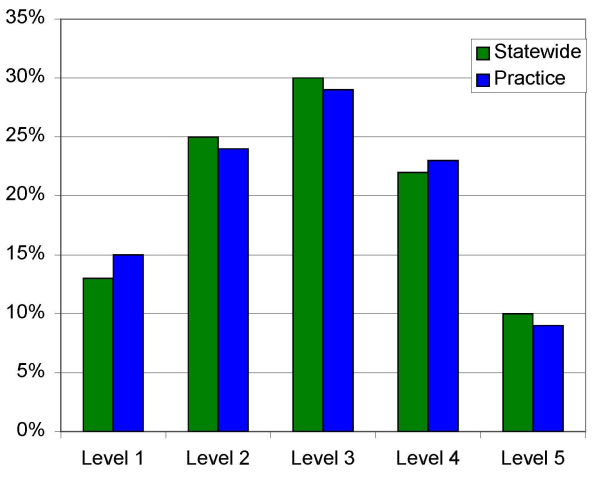
High-level E&M Codes Increase Risk of RAC Audit
Recovery Audit Contractors (RAC’s) are now reviewing high level evaluation and management (E&M) codes used in billing office visits in private practice. E&M services are based on the providers understanding of the patient’s medical history, review of patient’s medications, a physical examination, and of course a medical decision. According to Charles Fidel of AMedNews.com, Medicare paid $33.5 billion for E&M services in 2010. Of the 442,000 physicians that billed for E&M services, only 1,669 providers consistently billed high-level E&M codes such as 99215. A claim for a low-level visit by an established patient only paid about $20 in 2010, while a high-level new patient paid around $190.
Check Patient Eligibility For Wellness Visits To Ensure Reimbursement
Following on the heels of our recent article, “Billing and Coding for the Medicare Annual Wellness Visits,” we got this comment from a reader: