By Christine Moore, CPC -- There seems to be some confusion out there from both physician offices and patients as to what is included in the Medicare Wellness Visits. Office staff should be familiar with codes G0402, G0438, and G0439 to be able to explain to patients the purpose and scope of these visits. Medicare coverage includes three different types of Wellness Visits that are offered to all enrollees, but these visits do not include a routine physical checkup. They are intended to be a meeting between physician and patient to discuss current health status, and to devise a plan for maintaining good health, setting a schedule for preventive health screenings, and treating or stabilizing chronic ailments. Medicare beneficiaries are eligible to receive the services associated with the Wellness Visits at no charge to the patient, with no copay or deductible due for the Annual Wellness Visit (AWV) itself, but if other services are provided during the course of the AWV, the patient is responsible for any copay or deductible applicable to those extra services. Together, the three types of wellness visits are designed to establish and maintain regular contact between patient and physician, to ease communication about health and wellness issues, and to provide a basis for regular updating of patient records with regard to overall health. Each type of visit is indicated at a specific point during the term of the patient’s coverage under Medicare, and there are specific guidelines for time periods during which each visit is payable.
Medical Billing Blog
Billing and Coding For the Medicare Annual Wellness Visits
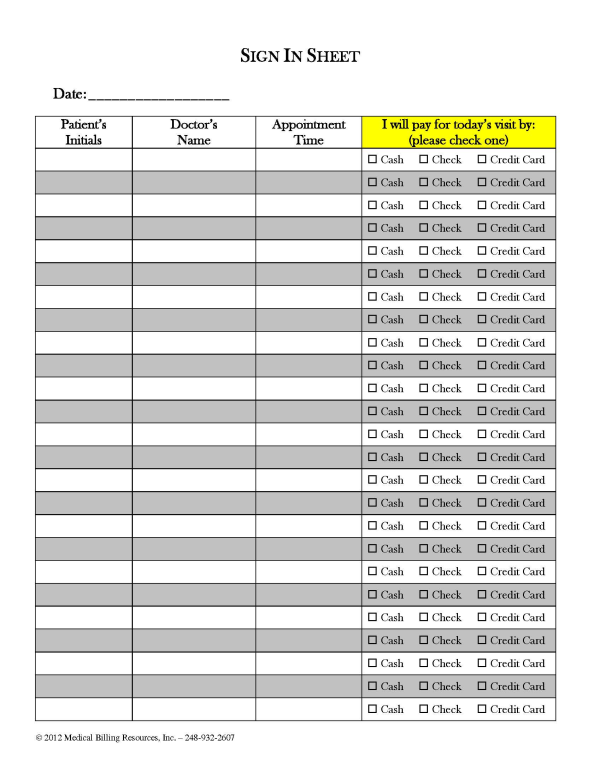
Easy Ways To Increase Front Desk Collections
As I’ve stated before, with a little extra effort on the part of your front desk staff, it’s easy to increase front desk collections and reduce patient receivables. Many front office personnel don’t like to ask for money at the time of service, but it becomes a little easier to begin the conversation with the help of the new sign in form we have designed, which brings up the topic of payment without your front desk staff having to say one word. Mind you, it’s still up to the provider or administrator to institute and enforce a new policy calling for this method of collection effort to be followed, but it does become less distasteful if staff approach the conversation with the help of this new tool.
How Medical Practices Can Reclaim Lost Revenue From Denials
What if I told you that you have been paying $48,000 a year, every year, for the privilege of chatting with your patients about their ailments, and treating them at no charge? You’d tell me I was off my rocker and that you’ve never done such a thing.
Maximize Reimbursement from Incident-To Billing
By Ralph Sitler III, JD -- Non-physician providers play an important role in medical practices these days, including nurse practitioners and a host of others. Understanding how Medicare recognizes these midlevel providers for reimbursement purposes is important for any practice utilizing their services. Compliance with Medicare guidelines for this type of billing is important if you want to be reimbursed correctly and stay on the right side of regulatory bodies.
Using Established Patient E/M Codes To Maximize Reimbursement
By Christina Hussan -- When a provider has not seen a patient for three or more years, it is permitted to bill for a new patient office visit. Actually, the time period is “three years plus one day,” to be exact, but the rules change when the patient has seen other providers in the group during the interim. It goes like this: If a patient has not seen any provider in a practice in three years (plus one day!), then it is appropriate to bill for a new patient office visit, but if any provider in the practice has seen the patient at any time within that three year period, it is required that the billing go through for an established patient visit.
Proper Use of Modifier 59 Can Increase Revenue for Medical Practices
By Heather Lakner, CPC -- Modifier 59 can be used in appropriate circumstances to unbundle codes to make them separately payable under Medicare guidelines. This can mean an increase in revenue for medical practices in circumstances when this modifier is appended correctly, with proper documentation to support its use. Unfortunately, Modifier 59 is often used incorrectly. Many billers will append it to a service to override an edit, but this can set up their medical practice for a substantial audit risk if it is applied incorrectly, or if cirumstances in the patient’s medical record do not clearly indicate that its use is appropriate.
Legal Issues To Consider When Implementing An EMR
Ralph Sitler III, JD--Many areas of industry welcome new technology with open arms, especially the medical field. Physicians and other health care professionals are always trying to find new and intrepid ways to improve patient care, increase efficiency, and boost the bottom line. However, there are often new risks associated with adopting new technology. This article aims to make physicians aware of some of these risks and help avoid potential legal issues concerning use of EMRs.
Include Documentation With Medical Billing Of Modifier 22
Karyn Shatzman, CPC, CGSC--Did you ever work really hard on something, above and beyond the normal circumstances, only to find out that you get no additional compensation for what you have accomplished? This happens to physicians all the time when they do medical billing for increased procedural services. The CPT book gives you a description of a service that is rendered by a physician. The American Medical Association, who writes the CPT, sets guidelines for that procedure code. What happens if that surgery that typically takes two hours to perform suddenly takes six hours? Maybe there were adhesions that the physician had to dissect for hours before they could even start the intended surgery. Payment schedules based on RVU’s do not take these circumstances into consideration, so modifier 22 was created.
Medical Billing E-prescribe Requirements for 2013
Medical Billing requirements for Medicare's e-prescribe program are different this year from previous years. To avoid the E-prescribe penalties in 2013, providers must successfully e-prescribe 10 times on eligible claims for service dates of January 1, 2012 through June 30, 2012 and that are processed by July 29, 2012. This means the claims must fully negotiate the Medicare system and be paid prior to July 29, 2012, so it’s of paramount importance that providers make sure they are processing enough eligible claims to avoid the penalty. Furthermore, we recommend that claims be submitted before the end of May, because Medicare traditionally begins holding claims in June so they can be paid in the third quarter. Note that this suggested submission date is not a deadline leveled by Medicare, and there is no guarantee that claims submitted by the end of May will be processed by the end of July. There is also no way to tell what other issues may come up with individual claims that may prevent them from being processed. Therefore, professionals should try to e-prescribe on more than 10 claims to ensure that they meet the quantity threshold.
Code Freeze Extends Through ICD-10 Implementation
Since HHS has proposed a year-long delay of implementing ICD-10, questions have been asked regarding the current ICD-9 code freeze. CMS confirmed that the code freeze will hold until ICD-10 is implemented, regardless of the delay, according to Pat Brooks, RHIA, and senior technical advisor at CMS.