The U.S. Department of Labor has issued a final rule that prohibits employers from requiring employees to wait more than 90 days after being hired before they can be covered by the Company’s sponsored health insurance plan.
Medical Billing Blog
DOL Issues Final Rule on Worker Eligibility for Health Insurance
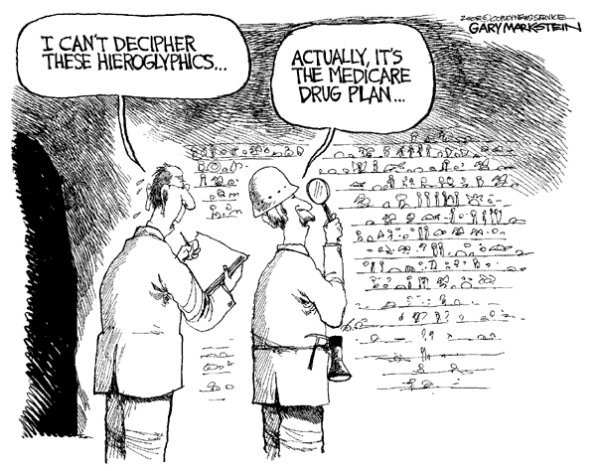
Proposed Medicare Part D Changes Are Postponed
The Obama administration has dropped plans to change the Medicare prescription drug program amid criticism from industry, patient advocacy groups and lawmakers that the changes would limit seniors’ access to certain medications and choice of plans. CMS Administrator Marilyn Tavenner wrote in a letter to Congress Monday that she was shelving changes proposed in January that could have loosened the requirements that Medicare Part D insurance plans cover a broad range of drugs in six “protected classes” of medications. Since the start of Medicare’s prescription drug benefit in 2006, the government has required insurers to cover “all or substantially all” drugs in six treatment areas. The administration proposed in January to lift the requirement for three types of medications: immunosuppressant drugs used in transplant patients; antidepressants; and antipsychotic medicines, used to treat schizophrenia and certain related disorders. Medicare officials had said the proposal would have saved money and reduced the overuse of drugs.
On February 6, the House Ways and Means Committee, House Energy and Commerce Committee, and Senate Finance Committee introduced a bi-partisan/bi-cameral bill to repeal the Medicare Sustainable Growth Rate (SGR) effective April 1, 2014. H.R. 4015. The Medicare Provider Payment Modernization Act consolidates three previously passed bills by each committee into a single framework to repeal and replace the flawed SGR.
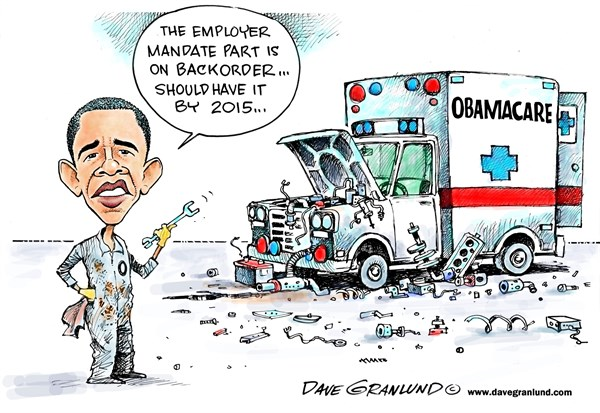
Obama Administration Unveils New Affordable Care Act Changes… again.
The Obama administration announced Wednesday that it has rewritten an array of far-reaching rules under the Affordable Care Act, the most significant of which will let people keep bare-bones health insurance policies for three more years. Americans with health insurance policies that don't meet consumer standards set by the president's healthcare law would be allowed to keep their plans into 2017, three years later than originally envisioned, so that people can buy these noncompliant plans through October 2016 and be covered by them until the following September, when Obama’s tenure in the White House will have ended. The healthcare law was designed to phase out health insurance plans in 2014 if they did not include a basic set of benefits and limits on how much consumers can be required to pay out of pocket for their medical care. After the controversy broke, the administration announced in November that state regulators could allow insurers to renew old policies in 2014. Only about half the states have agreed to the extensions. Some, particularly those with liberal, Democratic insurance regulators, have balked at allowing what they consider substandard plans to remain on the market.
In late February, CMS announced a temporary suspension of NEW RAC audits, effective February 21st. The Recovery Audit Contractors (RACs) currently under contract to CMS were directed to discontinue sending post-payment Additional Documentation Requests (ADRs) to providers until further notice.
Now Available: Subsidies for Insurance Policies Bought Outside Exchange
With just a month left for Americans to select health plans this year through new insurance marketplaces, the Obama administration is bending some rules to prevent people from being stranded without coverage, especially those in states where their own state-run online exchange has failed disastrously. The new policy applies to people who — because of “technical issues” — were prevented in trying to buy insurance through an online exchange and signed up for a health plan outside the marketplace. They will now be allowed to sign up for coverage in the exchange and get federal subsidies “on a retroactive basis,” going back to the date on which they first enrolled in a health plan outside the exchange. The state-run exchanges in some of these states — Oregon, Maryland, Massachusetts and Hawaii in particular — have experienced more technical problems than even the federal website. Consumers in those states are still having difficulty enrolling five months after the launch. Federal officials said they had agreed to provide such assistance retroactively because technical problems had prevented consumers from using online exchanges to obtain insurance and financial aid in some states. The Obama administration’s decision came as a surprise because the Affordable Care Act is clear: Federal subsidies are available only to people who enroll in a “qualified health plan” through an exchange. The HHS change will allow those who tried to sign up on their state-run exchanges, but couldn’t, to retroactively obtain the subsidies they would have been eligible for, even if they ended up purchasing healthcare through a private insurer. The privately purchased plans must still meet certain basic requirements of the healthcare law.
There will be no more delays to the October 1 deadline to implement the International Classification of Diseases-10th revision (ICD-10) coding system.
Marketplace Enrollment Update: February 2014
Enrollment in health plans sold on marketplaces created by President Obama’s health care law has hit 4 million, the administration announced Tuesday, marking another milestone in the law’s implementation. The number suggests sign-ups have continued at a brisk pace in February, with about 700,000 people selecting an insurance plan so far this month. And with five weeks before the enrollment period deadline at the end of March, they put the administration on pace to come close to the Congressional Budget Office's initial projection that 7 million individuals would sign up for insurance coverage during the period. Health officials continue to see “strong demand nationwide” and that more than 12 million calls have come into the federal call center since the fall. But with the good news remain some questions. The number of people who have signed up for plans and paid their first month's premium remains unknown, though insurers have suggested about 20 percent of individuals have not paid. Moreover, it is unclear how many of those individuals who signed up in February were young and healthy -- the population demographic that the administration needs to ensure that the exchanges have a stable balance of healthy and sick consumers. A senior administration official said that a more detailed report about the enrollees would be released in mid-March.
Major Spending Cut Proposed For Medicare Advantage
The Obama administration is proposing a major cut in 2015 payments to Medicare Advantage. An annual notice released Friday after the markets closed would reduce Medicare Advantage spending by 3.55 percent. The CMS based its projections, which will differ across the country based on a variety of factors, on an expected 3.55% decline in the Medicare Advantage growth rate factor and an expected decline of 1.65% in per capita expenditures in the fee-for-service portion of the senior citizen healthcare program. The annual rate adjustment — which is only one of the payment changes — is calculated through a complicated set of formulas, and analysts were still sorting out the 148-page proposal that CMS released late in the afternoon to assess the total impact on the increasingly popular program for seniors. The cut is bigger than the industry expected, given estimates the government provided in December. Last year, the administration proposed 2.2 percent in cuts for Medicare Advantage plans. After a six-week campaign that included paid advertising inside the Beltway and beyond, and letters from at least 160 supportive lawmakers from both parties, CMS reversed a key assumption that had long been built into its estimates and instead put forward a 3.3 percent growth rate. According to a new analysis from consulting firm Avalere Health, enrollment in Medicare Advantage plans rose in 2014 by 8.9 percent to 15.9 million enrollees, up from 14.6 million in 2013. Approximately 30 percent of Medicare beneficiaries are enrolled in the plans, which are offered by private insurance companies.
Twenty-five people were charged Thursday with obtaining at least $75 million in fraudulent Medicaid payments from the District of Columbia government, a series of cases that federal prosecutors said added up to the largest health-care fraud in the city’s history. U.S. Attorney Ronald C. Machen Jr. said agents fanned out across the D.C. region to make arrests and seize six luxury vehicles and 49 bank accounts, capping off a multiyear investigation. Prosecutors said personal health care in private homes is a thriving front in Medicaid fraud, a category of Medicaid claims that has grown dramatically in the city over the past 8 years, and said there have been similar cases out of Miami and Detroit. The uptick in billings for home care — from $40 million in 2006 to $280 million last year — was part of what tipped off authorities to illegal activity, U.S. Attorney Ronald Machen said. Prosecutors say many of the defendants persuaded patients to fake illness or injury so they could bill Medicaid for home care they didn’t receive. Some of those patients received kickbacks, authorities said, although no patients have been charged. Those charged include the owners of home-care firms and nurse staffing agencies, home-care aides and recruiters who signed up patients.