The federal government may not completely finish the automated payment system for Healthcare.gov for “several months,” White House spokesman Jay Carney said Friday. Until that system is fully running, the administration won’t be able to verify how many of the consumers who signed up for through the health insurance website are, in fact, paying their premiums and are hence truly enrolled. The administration reported earlier in the week that nearly 3.3 million people have selected plans on through the marketplace as of Feb. 1. However, insurance companies are saying that about 20 percent of those people failed to pay their premiums on time and consequently didn’t receive coverage in January, the New York Times reports. Paying the first month’s premium is the final step in completing an enrollment. Under federal rules, people must pay the initial premium to have coverage take effect. In view of the chaotic debut of the federal marketplace and many state exchanges, the White House urged insurers to give people more time, and many agreed to do so. But, insurers said, some people missed even the extended deadlines.
Medical Billing Blog
Healthcare.gov's Payment System Months from Completion
At its January meeting, the Medicare Payment Advisory Commission (MedPAC) voted unanimously to approve a recommendation to Congress that the differences in payments between outpatient departments and physician offices for 66 Ambulatory Payment Classifications (APCs) be reduced or eliminated. The services include imaging, procedures such as small-intestine endoscopy, tests including bone density tests and other kinds of care. The change would mean a 0.6% drop in Medicare revenue for hospitals.
On January 17th, CMS announced a new policy regarding Freedom of Information Act (FOIA) requests for the disclosure of how much Medicare pays individual physicians. For the past 30 years, this information has been protected from FOIA requests under the Personal Privacy Exemption (Exemption 6) of the act. Under the new policy,CMS will begin examining each FOIA request on a case-by-case basis to determine if the information requested should be exempt from FOIA requests.
Obama Administration Delays Part Of Employer Mandate Again
The Obama administration announced Monday it would give medium-sized employers an extra year, until 2016, before they must offer health insurance to their full-time workers. Firms with at least 100 employees will have to start offering this coverage in 2015. Small businesses with fewer than 50 workers have always been exempt from the new coverage requirements but the law originally required all other businesses to start covering their workers for face penalties beginning Jan. 1, 2014. Under the Affordable Care Act, larger employers are generally subject to tax penalties if they fail to offer "minimum essential coverage" to full-time employees and their dependents. The administration laid out a three-tier approach. For larger employers with 100 or more employees (about 2 percent of employers): Seventy percent of employees must be offered coverage in 2015, and in later years at least 95 percent of employees must be offer coverage. Employers that do not meet these standards will be subject to tax penalties. For employers with 50 to 99 employees (about 2 percent of employers): Companies with 50 to 99 employees will have an extra year, until 2016, to provide coverage or pay tax penalties. For small businesses with fewer than 50 employees (about 96 percent of all employers): These companies will not be required to provide coverage or fill out any forms in any year. Officials Monday said that the delay in the Affordable Care Act mandate will affect 50 percent of the businesses that were supposed to be complying by 2015. About 7.8 million workers are employed by the affected businesses. However, those officials also took pains to note that the so-called employer mandate to offer affordable health insurance to workers does not affect 96 percent of the employers in the U.S., because they have fewer than 50 full-time employees.
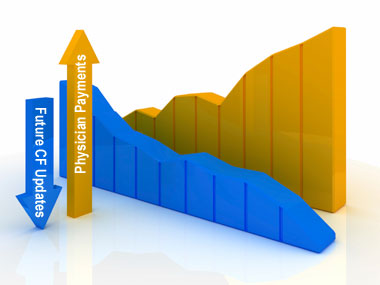
Update: Sustainable Growth Rate (SGR) Reform
On Thursday afternoon (2/6) the House Ways and Means Committee, House Energy and Commerce Committee, and Senate Finance Committee leadership introduced a bi-partisan/bi-cameral bill to repeal and replace the Medicare Sustainable Growth Rate (SGR) formula. The Congressional sponsors have provided a section-by-section summary for your review.
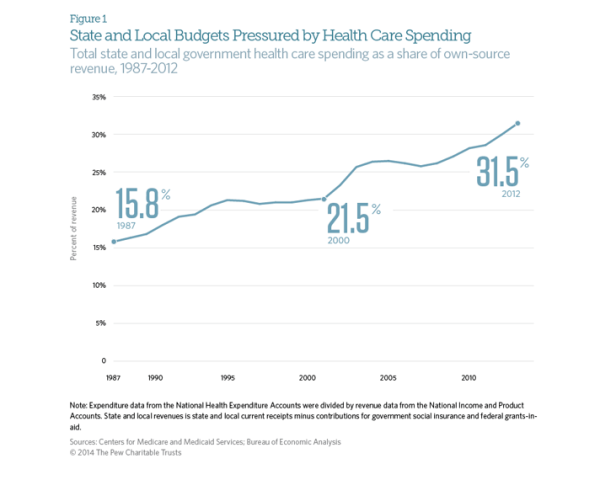
State and Local Governments Spend 31.5% on Healthcare
The Affordable Care Act was supposed to stem the rapidly rising cost of healthcare in the United States. While costs have continued to rise since the ACA’s passage in 2010, the rate has slowed dramatically. Early indicators suggest that the growth rate of total healthcare spending in the US was only 4% in 2012. This is an improvement when looking at the aggregate expenditures, unfortunately, for state and local governments, the cost curve has not had any form of reduction. According to CMS and the Bureau of Economic Analysis, state and local governments spent 31.5% of their budgets on healthcare costs in 2012. That represents an 8 percent increase over the previous year, or a rate twice as fast as the national rate of increase. This increase is largely due in part to the stimulus bill passed by Congress in 2009. The American recovery and Reinvestment Act granted more than $100 billion to states to cover increasing Medicaid costs, which had ballooned during the recession as high unemployment drove job-seekers to the government run health program. During this period, even though Medicaid saw increased participants, overall state spending on Mediciad actually fell. However, the federal stimulus money would not last forever and State Mediciad expenditures rose 22 percent between 2010 and 2011, and another 15 percent in 2012. The Government Accountability Office says health-care spending represents the single greatest threat to state and local government long-term health.
City of Detroit and Retirees Reach Agreement on Health Insurance
The city of Detroit and its retirees have reached an agreement in a health insurance dispute that may end a lawsuit against the city. Retirees filed suit in November to stop the city from shifting them to Medicare and giving those under age 65 a $125 monthly stipend to buy their own insurance. The parties reached an agreement in principle Thursday night covering benefits through the end of 2014, mediators in Detroit's bankruptcy said Friday in a statement. Some features of the deal include the increase to $300 in the monthly stipend for retirees over age 65 who aren't eligible for Medicare. The stipend for retirees under age 65 will be increased to $175 if the household income is less than $75,000 and the retiree acquires insurance under a health care exchange. The stipend is $50 more than the amount proposed last year by emergency manager Kevyn Orr. A lawsuit retiree groups filed in bankruptcy court Jan. 9 challenging the city’s plan to slash benefits will be dismissed as a result of the settlement, according to a statement from the Detroit bankruptcy court mediators.
Marketplace Enrollment Update: January 2014
Approximately 3 million people have now enrolled in health insurance plans sold through marketplaces created by President Obama’s health law, the administration announced Friday. The milestone indicates nearly a million additional people have signed up since the end of December. It also suggests that the marketplaces are continuing to recover from a disastrous launch on Oct. 1. That still leaves the Obama administration lagging behind its initial projections for overall health law enrollment--but also closer to hitting monthly sign-up expectations it set back in September. The numbers are reassuring for supporters of the Affordable Care Act, who were worried that the pace of sign-ups for private plans would slow in January and February, before picking up again as the March 31 enrollment deadline for 2014 coverage approached. But they are still shy of initial projections from the Centers for Medicare and Medicaid Services, which originally expected 4.4 million people to sign up for a plan by the end of January. Moreover, the administration has not provided data on how many of the people who have signed up for plans through the exchanges have actually made a payment, which is required to ensure coverage.
The Office of the National Coordinator for Health Information Technology has finally released SAFER Guides, a series of nine guidance documents that help EHR operators to use the technology safely in a variety of areas. The nine documents are organized into three broad categories – foundational guides, infrastructure guides and clinical process guides. They are all downloadable in an easy to view PDF format or they can be accessed through the website’s interactive tool. Both options are available at the following address: http://www.healthit.gov/policy-researchers-implementers/safer.
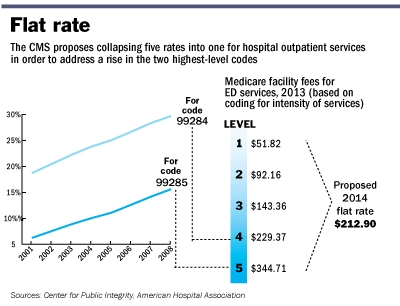
CMS issues 2014 Outpatient Facility Policy and Payment Changes
Last November, CMS released a final CY 2014 hospital outpatient and ambulatory surgical center (ASC) payment Final Rule. Most significantly, “CMS will replace the current five levels of hospital clinic visit codes for both new and established patients with a single code describing all outpatient clinic visits.” CMS believes that a single code and payment is administratively simpler for hospitals and “better reflects hospital resources involved in supporting an outpatient visit.”