On December 13,CMS released the Physician Quality Reporting System (PQRS) measure documents for 2014. You are advised that some of these measures may be different from the PQRS measure documents of prior years.
Medical Billing Blog
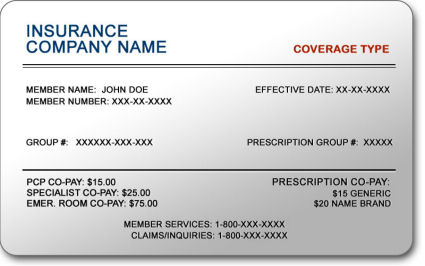
Verifying Patient Coverage in a Health Insurance Marketplace Plan
Beginning January 1, 2014, providers will be verifying their patient’s insurance status when they show up for their appointments. Many of these patients may be newly insured individuals who will be getting their health insurance through the Health Insurance Marketplace, also known as Health Insurance Exchange.
MBR Explains: Quality Improvements - Key Features of the ACA by Year -- 2011
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2011 that sought to improve quality and lower cost of healthcare. The majority of these changes effected seniors enrolled in Medicare. The ACA aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key quality improvement provisions that took effect in 2011.
Health Insurance in 2014: Lower Premiums but Higher Deductibles
Details are now available on the costs associated with health plans being offered through Healthcare.gov, and some people are finding their insurance will cost more than they had hoped. Until last week, the federal government blocked users from viewing deductible amounts associated with available health plans, limiting consumers to view only premium and copayment amounts. Insurers assumed consumers would pick plans mainly on price, as reflected in the monthly premium, so it was to their advantage, as well as to the government’s, that consumers were unable to view a plan’s annual deductible, or the amount consumers need to pay before coverage kicks in. The federal government finally relented and allowed consumers to basically ‘window shop’ for coverage. For policies offered in the federal exchange, the annual deductible often tops $5,000 for an individual and $10,000 for a couple. The average individual deductible for what is called a bronze plan on the exchange is $5,081 a year, according to a new report on insurance offerings in 34 of the 36 states that are relying on the federally run marketplace. While the costs of these plans are surprising many, they are more generous than what is currently available in the individual market. However, the plans are significantly less generous than what most employers are providing, creating a sticker shock sensation to consumers that are no longer receiving employer-sponsored health insurance.
Healthcare.gov Enrollment Numbers Start to Rise
Centers for Medicare and Medicaid Services (CMS) released its 2014 Medicare physician fee schedule (PFS) Final Rule. CMS calculates the 2014 Physician Fee Schedule Conversion Factor (CF) to be $27.2006, or a 20.1% reduction from the current CF of $34.0230. Total payments under the fee schedule in 2014 are projected to be at $87 billion, according to CMS. Payments to physicians are calculated primarily on three key factors: the resource-based relative value scale (RBRVS), the geographic practice cost indexes (GPCIs), and the monetary conversion factor (CF).
MBR Explains: Increasing Access - Key Features of the Affordable Care Act by Year -- 2010
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2010 that sought to increase access to affordable healthcare. As previously mentioned, the Patient Protection and Affordable Care Act was signed by President Obama on March 23, 2010. The law aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key provisions aimed to increase access that took effect in 2010.
MBR Explains: The Hospital Value-Based Purchasing Program
Historically, the United Stateshas paid for its healthcare under a fee-for-service (FFS) model. Every visit, test, procedure, and consultation receives an individual fee. It incentivizes volume over quality. It discourages integrated care. And it contributes toAmerica’s high health care expenditures. There have been many attempts to reform our payment system – bundled payments, capitation, episode of care payment, comprehensive care payment – but as of 2009, no state has successfully eliminated the FFS system.
MBR Explains: Quality Improvements - Key Features of the Affordable Care Act by Year -- 2010
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2010 that sought to improve quality and lower cost of healthcare. As previously mentioned, the Patient Protection and Affordable Care Act was signed by President Obama on March 23, 2010. The law aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key quality improvement provisions that took effect in 2010.