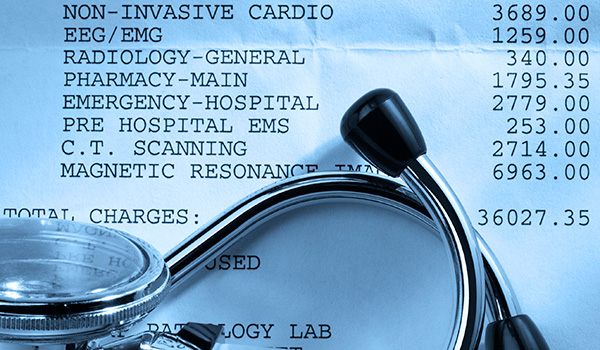
The American Medical Association issued a statement to physicians on Wednesday cautioning doctors on how to navigate a 90-day grace period for government-subsidized health plans. A patient with subsidized insurance who is falling behind in payments is guaranteed coverage for medical bills for 30 days – but insurers can ultimately deny payment during the remaining 60 days. Some doctors and the AMA say insurance companies could delay and then retroactively deny claims made during the 60-day period – a bill then held stuck with physicians.
Medical Billing Blog
Doctors Say Grace Period Will Leave Them With Unpaid Bills
Kathleen Sebelius, the secretary of health and human services, said Wednesday that the Obama administration would not extend the deadline for people to sign up for health insurance or delay the requirement for most Americans to have coverage. There will also be no delay in the penalty most Americans face under President Barack Obama's healthcare reform law if they fail to obtain health coverage this year. Last year, embracing nonpartisan estimates for the Affordable Care Act, Health and Human Services Secretary Kathleen Sebelius set a benchmark for the new insurance marketplaces: "Success looks like at least 7 million people having signed up by the end of March 2014," she said to NBC. Enrollment, however, began at a terribly slow pace in October because of all the technical problems with HealthCare.gov, the federal health exchange website serving 36 states. Some state-run health exchange websites have had their own problems as well. Within that context, Sebelius on Wednesday redefined what success looks like: "Success looks like millions of people with affordable health coverage, which we will have by the end of March," she told the House Ways and Means Committee. The administration released the latest enrollment figures on Tuesday—revealing that some 4.2 million Americans have signed up for coverage on the new exchanges. However, that figure does not include how many people have actually paid for their plans—a metric that could make the actual number of enrollees significantly lower.
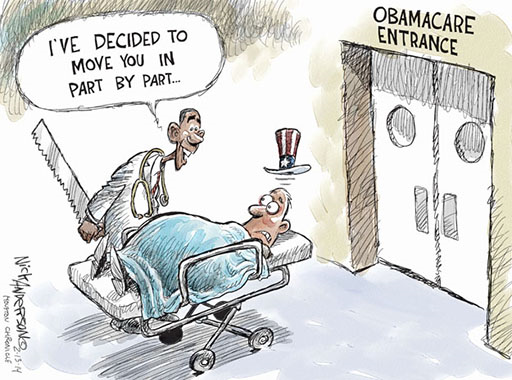
Obama Administration Unveils New Affordable Care Act Changes… again.
The Obama administration announced Wednesday that it has rewritten an array of far-reaching rules under the Affordable Care Act, the most significant of which will let people keep bare-bones health insurance policies for three more years. Americans with health insurance policies that don't meet consumer standards set by the president's healthcare law would be allowed to keep their plans into 2017, three years later than originally envisioned, so that people can buy these noncompliant plans through October 2016 and be covered by them until the following September, when Obama’s tenure in the White House will have ended. The healthcare law was designed to phase out health insurance plans in 2014 if they did not include a basic set of benefits and limits on how much consumers can be required to pay out of pocket for their medical care. After the controversy broke, the administration announced in November that state regulators could allow insurers to renew old policies in 2014. Only about half the states have agreed to the extensions. Some, particularly those with liberal, Democratic insurance regulators, have balked at allowing what they consider substandard plans to remain on the market.
Now Available: Subsidies for Insurance Policies Bought Outside Exchange
With just a month left for Americans to select health plans this year through new insurance marketplaces, the Obama administration is bending some rules to prevent people from being stranded without coverage, especially those in states where their own state-run online exchange has failed disastrously. The new policy applies to people who — because of “technical issues” — were prevented in trying to buy insurance through an online exchange and signed up for a health plan outside the marketplace. They will now be allowed to sign up for coverage in the exchange and get federal subsidies “on a retroactive basis,” going back to the date on which they first enrolled in a health plan outside the exchange. The state-run exchanges in some of these states — Oregon, Maryland, Massachusetts and Hawaii in particular — have experienced more technical problems than even the federal website. Consumers in those states are still having difficulty enrolling five months after the launch. Federal officials said they had agreed to provide such assistance retroactively because technical problems had prevented consumers from using online exchanges to obtain insurance and financial aid in some states. The Obama administration’s decision came as a surprise because the Affordable Care Act is clear: Federal subsidies are available only to people who enroll in a “qualified health plan” through an exchange. The HHS change will allow those who tried to sign up on their state-run exchanges, but couldn’t, to retroactively obtain the subsidies they would have been eligible for, even if they ended up purchasing healthcare through a private insurer. The privately purchased plans must still meet certain basic requirements of the healthcare law.
Marketplace Enrollment Update: February 2014
Enrollment in health plans sold on marketplaces created by President Obama’s health care law has hit 4 million, the administration announced Tuesday, marking another milestone in the law’s implementation. The number suggests sign-ups have continued at a brisk pace in February, with about 700,000 people selecting an insurance plan so far this month. And with five weeks before the enrollment period deadline at the end of March, they put the administration on pace to come close to the Congressional Budget Office's initial projection that 7 million individuals would sign up for insurance coverage during the period. Health officials continue to see “strong demand nationwide” and that more than 12 million calls have come into the federal call center since the fall. But with the good news remain some questions. The number of people who have signed up for plans and paid their first month's premium remains unknown, though insurers have suggested about 20 percent of individuals have not paid. Moreover, it is unclear how many of those individuals who signed up in February were young and healthy -- the population demographic that the administration needs to ensure that the exchanges have a stable balance of healthy and sick consumers. A senior administration official said that a more detailed report about the enrollees would be released in mid-March.
Healthcare.gov's Payment System Months from Completion
The federal government may not completely finish the automated payment system for Healthcare.gov for “several months,” White House spokesman Jay Carney said Friday. Until that system is fully running, the administration won’t be able to verify how many of the consumers who signed up for through the health insurance website are, in fact, paying their premiums and are hence truly enrolled. The administration reported earlier in the week that nearly 3.3 million people have selected plans on through the marketplace as of Feb. 1. However, insurance companies are saying that about 20 percent of those people failed to pay their premiums on time and consequently didn’t receive coverage in January, the New York Times reports. Paying the first month’s premium is the final step in completing an enrollment. Under federal rules, people must pay the initial premium to have coverage take effect. In view of the chaotic debut of the federal marketplace and many state exchanges, the White House urged insurers to give people more time, and many agreed to do so. But, insurers said, some people missed even the extended deadlines.
On January 17th, CMS announced a new policy regarding Freedom of Information Act (FOIA) requests for the disclosure of how much Medicare pays individual physicians. For the past 30 years, this information has been protected from FOIA requests under the Personal Privacy Exemption (Exemption 6) of the act. Under the new policy,CMS will begin examining each FOIA request on a case-by-case basis to determine if the information requested should be exempt from FOIA requests.
Obama Administration Delays Part Of Employer Mandate Again
The Obama administration announced Monday it would give medium-sized employers an extra year, until 2016, before they must offer health insurance to their full-time workers. Firms with at least 100 employees will have to start offering this coverage in 2015. Small businesses with fewer than 50 workers have always been exempt from the new coverage requirements but the law originally required all other businesses to start covering their workers for face penalties beginning Jan. 1, 2014. Under the Affordable Care Act, larger employers are generally subject to tax penalties if they fail to offer "minimum essential coverage" to full-time employees and their dependents. The administration laid out a three-tier approach. For larger employers with 100 or more employees (about 2 percent of employers): Seventy percent of employees must be offered coverage in 2015, and in later years at least 95 percent of employees must be offer coverage. Employers that do not meet these standards will be subject to tax penalties. For employers with 50 to 99 employees (about 2 percent of employers): Companies with 50 to 99 employees will have an extra year, until 2016, to provide coverage or pay tax penalties. For small businesses with fewer than 50 employees (about 96 percent of all employers): These companies will not be required to provide coverage or fill out any forms in any year. Officials Monday said that the delay in the Affordable Care Act mandate will affect 50 percent of the businesses that were supposed to be complying by 2015. About 7.8 million workers are employed by the affected businesses. However, those officials also took pains to note that the so-called employer mandate to offer affordable health insurance to workers does not affect 96 percent of the employers in the U.S., because they have fewer than 50 full-time employees.
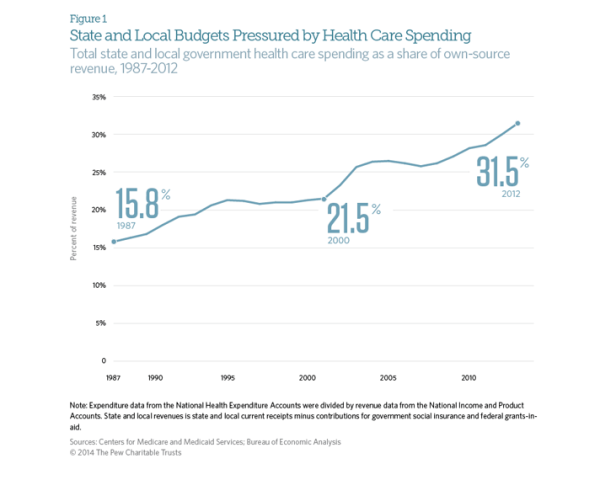
State and Local Governments Spend 31.5% on Healthcare
The Affordable Care Act was supposed to stem the rapidly rising cost of healthcare in the United States. While costs have continued to rise since the ACA’s passage in 2010, the rate has slowed dramatically. Early indicators suggest that the growth rate of total healthcare spending in the US was only 4% in 2012. This is an improvement when looking at the aggregate expenditures, unfortunately, for state and local governments, the cost curve has not had any form of reduction. According to CMS and the Bureau of Economic Analysis, state and local governments spent 31.5% of their budgets on healthcare costs in 2012. That represents an 8 percent increase over the previous year, or a rate twice as fast as the national rate of increase. This increase is largely due in part to the stimulus bill passed by Congress in 2009. The American recovery and Reinvestment Act granted more than $100 billion to states to cover increasing Medicaid costs, which had ballooned during the recession as high unemployment drove job-seekers to the government run health program. During this period, even though Medicaid saw increased participants, overall state spending on Mediciad actually fell. However, the federal stimulus money would not last forever and State Mediciad expenditures rose 22 percent between 2010 and 2011, and another 15 percent in 2012. The Government Accountability Office says health-care spending represents the single greatest threat to state and local government long-term health.
Marketplace Enrollment Update: January 2014
Approximately 3 million people have now enrolled in health insurance plans sold through marketplaces created by President Obama’s health law, the administration announced Friday. The milestone indicates nearly a million additional people have signed up since the end of December. It also suggests that the marketplaces are continuing to recover from a disastrous launch on Oct. 1. That still leaves the Obama administration lagging behind its initial projections for overall health law enrollment--but also closer to hitting monthly sign-up expectations it set back in September. The numbers are reassuring for supporters of the Affordable Care Act, who were worried that the pace of sign-ups for private plans would slow in January and February, before picking up again as the March 31 enrollment deadline for 2014 coverage approached. But they are still shy of initial projections from the Centers for Medicare and Medicaid Services, which originally expected 4.4 million people to sign up for a plan by the end of January. Moreover, the administration has not provided data on how many of the people who have signed up for plans through the exchanges have actually made a payment, which is required to ensure coverage.