Chances are that you like all the members of your staff, and that you appreciate their integrity, loyalty and hard work; so the thought that one of them could be stealing from you is probably not at the top of your list of things to worry about today. But if you’re leaving everything to your staff while you focus on patient care, you might very well be tempting them with an irresistible carrot.
Medical Billing Blog
Most medical offices have procedures in place that attempt to address the inevitable cases of last-minute cancellations and patient no shows. There are a number of tricks to handling them effectively to minimize their frequency and the damage they can do to the practice’s revenue in general. After all, a medical practice is a business, and the best business solutions are those that yield the greatest positive effect with the lowest overall cost financially and with the least effort. In the case of patient no shows, it is important to realize why and when they occur in order to devise the best combination of ways to respond to them and mitigate their effect on the schedule—and your revenue—over all.
Check Patient Eligibility For Wellness Visits To Ensure Reimbursement
Following on the heels of our recent article, “Billing and Coding for the Medicare Annual Wellness Visits,” we got this comment from a reader:
In a recently published article by Ricardo Alonso Zaldivar, reporting for the Associate Press, our healthcare system wastes $750 billion a year. Almost 30 cents of every dollar is spent on unneeded care, paperwork, and fraud, according to the Institute of Medicine.
The federal government has finalized a one-year delay for the nationwide conversion to ICD-10 code sets beginning Oct. 1, 2014. HHS Secretary Kathleen Sebelius has announced a final rule establishing a one-year delay - from Oct. 1, 2013, to Oct. 1, 2014 in the use of the ICD-10 Coding system.
Meaningful Use Stage 2 Requirement Changes
On Thursday, August 23, 2012, U.S. Department of Health and Human Services Secretary Kathleen Sebelius announced that the Centers for Medicare & Medicaid Services (CMS) published the final rule for Stage 2 Meaningful Use for the Electronic Health Record (EHR) Incentive Programs. The rule provides new criteria that eligible professionals (EPs), eligible hospitals, and critical access hospitals (CAHs) must meet in order to successfully participate in the EHR Incentive Programs.
For most practices, the process of adopting and implementing an Electronic Health Record System is daunting enough. It can take as long as a year to fully integrate the EHR into the daily procedures of the practice, and most practices find themselves on a whirlwind roller coaster ride when it comes to devising and fine-tuning new routines to make using the EHR as effectively as possible. In the long run, switching to electronic records is worth it in terms of time saved, errors reduced, and being able to offer the additional soft services available from those who use an electronic record system.
Where Should I Send My Bill? Treating Young Adults (Part 3 of 3)
Ralph Sitler III, J.D. -- In the first two installments of this blog series, we covered some fundamental principles that deal with providing care to minors, obtaining appropriate authorization to provide the care, and how to determine who is responsible to pay for the services rendered. As discussed, it’s not always the parent or guardian of the minor obtaining services.
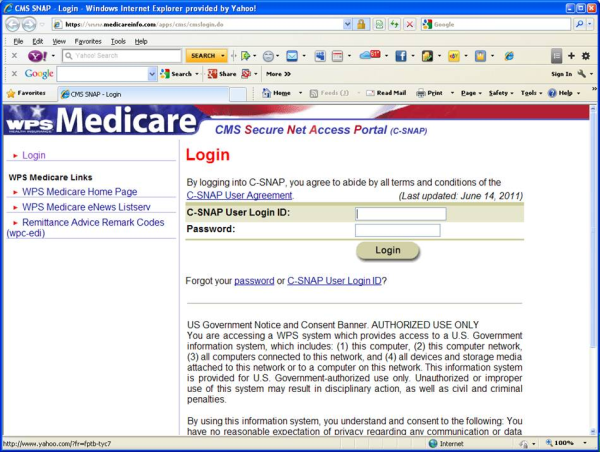
CMS Starts Meaningful Use Audits for EMR Adopters
Under the 2009 federal economic stimulus package, health care providers who demonstrate meaningful use of a certified electronic health record system qualify for Medicare or Medicaid incentive programs.
Who Pays For Services Provided To Minors? (Part 2 of 3)
By Ralph Sitler III, JD -- Last week, we discussed why it’s important for providers to consider the type of service rendered to minors when determining who has authority to contract that service, and how to determine who bears financial responsibility to pay for those services under various conditions. Essentially, we covered what types of services minors can authorize on their own behalf, and whom to bill for the services. We also discussed some pretty serious considerations to take into account when submitting claims to an insurance plan for reimbursement of services self-authorized by minors when the insurance plan policy holder is the minor’s parent or guardian. HIPAA guidelines are a little vague when it comes to notification of other individuals when a minor has self-authorized, so be sure to check out that first blog in this series to make sure you’re up to date on the guidelines.