At its January meeting, the Medicare Payment Advisory Commission (MedPAC) voted unanimously to approve a recommendation to Congress that the differences in payments between outpatient departments and physician offices for 66 Ambulatory Payment Classifications (APCs) be reduced or eliminated. The services include imaging, procedures such as small-intestine endoscopy, tests including bone density tests and other kinds of care. The change would mean a 0.6% drop in Medicare revenue for hospitals.
Medical Billing Blog
On January 17th, CMS announced a new policy regarding Freedom of Information Act (FOIA) requests for the disclosure of how much Medicare pays individual physicians. For the past 30 years, this information has been protected from FOIA requests under the Personal Privacy Exemption (Exemption 6) of the act. Under the new policy,CMS will begin examining each FOIA request on a case-by-case basis to determine if the information requested should be exempt from FOIA requests.
Update: Sustainable Growth Rate (SGR) Reform
On Thursday afternoon (2/6) the House Ways and Means Committee, House Energy and Commerce Committee, and Senate Finance Committee leadership introduced a bi-partisan/bi-cameral bill to repeal and replace the Medicare Sustainable Growth Rate (SGR) formula. The Congressional sponsors have provided a section-by-section summary for your review.
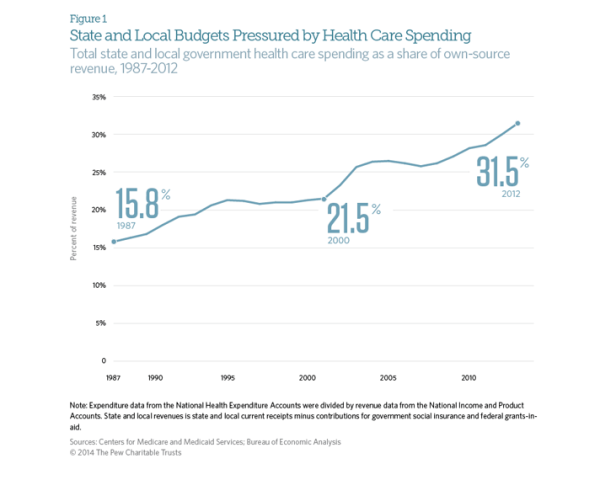
State and Local Governments Spend 31.5% on Healthcare
The Affordable Care Act was supposed to stem the rapidly rising cost of healthcare in the United States. While costs have continued to rise since the ACA’s passage in 2010, the rate has slowed dramatically. Early indicators suggest that the growth rate of total healthcare spending in the US was only 4% in 2012. This is an improvement when looking at the aggregate expenditures, unfortunately, for state and local governments, the cost curve has not had any form of reduction. According to CMS and the Bureau of Economic Analysis, state and local governments spent 31.5% of their budgets on healthcare costs in 2012. That represents an 8 percent increase over the previous year, or a rate twice as fast as the national rate of increase. This increase is largely due in part to the stimulus bill passed by Congress in 2009. The American recovery and Reinvestment Act granted more than $100 billion to states to cover increasing Medicaid costs, which had ballooned during the recession as high unemployment drove job-seekers to the government run health program. During this period, even though Medicaid saw increased participants, overall state spending on Mediciad actually fell. However, the federal stimulus money would not last forever and State Mediciad expenditures rose 22 percent between 2010 and 2011, and another 15 percent in 2012. The Government Accountability Office says health-care spending represents the single greatest threat to state and local government long-term health.
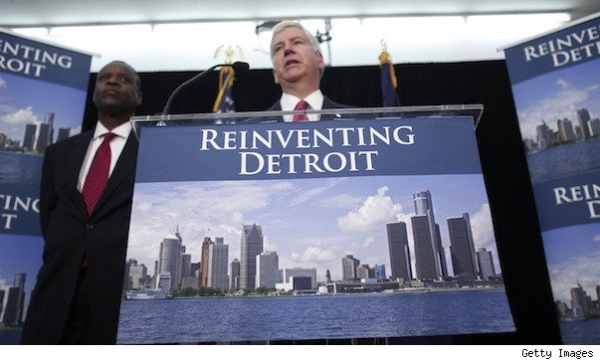
City of Detroit and Retirees Reach Agreement on Health Insurance
The city of Detroit and its retirees have reached an agreement in a health insurance dispute that may end a lawsuit against the city. Retirees filed suit in November to stop the city from shifting them to Medicare and giving those under age 65 a $125 monthly stipend to buy their own insurance. The parties reached an agreement in principle Thursday night covering benefits through the end of 2014, mediators in Detroit's bankruptcy said Friday in a statement. Some features of the deal include the increase to $300 in the monthly stipend for retirees over age 65 who aren't eligible for Medicare. The stipend for retirees under age 65 will be increased to $175 if the household income is less than $75,000 and the retiree acquires insurance under a health care exchange. The stipend is $50 more than the amount proposed last year by emergency manager Kevyn Orr. A lawsuit retiree groups filed in bankruptcy court Jan. 9 challenging the city’s plan to slash benefits will be dismissed as a result of the settlement, according to a statement from the Detroit bankruptcy court mediators.
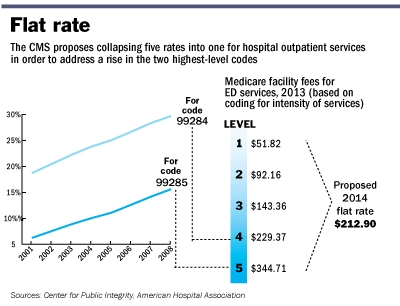
CMS issues 2014 Outpatient Facility Policy and Payment Changes
Last November, CMS released a final CY 2014 hospital outpatient and ambulatory surgical center (ASC) payment Final Rule. Most significantly, “CMS will replace the current five levels of hospital clinic visit codes for both new and established patients with a single code describing all outpatient clinic visits.” CMS believes that a single code and payment is administratively simpler for hospitals and “better reflects hospital resources involved in supporting an outpatient visit.”
MBR Explains: Quality Improvements - Key Features of the ACA by Year -- 2011
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2011 that sought to improve quality and lower cost of healthcare. The majority of these changes effected seniors enrolled in Medicare. The ACA aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key quality improvement provisions that took effect in 2011.
Centers for Medicare and Medicaid Services (CMS) released its 2014 Medicare physician fee schedule (PFS) Final Rule. CMS calculates the 2014 Physician Fee Schedule Conversion Factor (CF) to be $27.2006, or a 20.1% reduction from the current CF of $34.0230. Total payments under the fee schedule in 2014 are projected to be at $87 billion, according to CMS. Payments to physicians are calculated primarily on three key factors: the resource-based relative value scale (RBRVS), the geographic practice cost indexes (GPCIs), and the monetary conversion factor (CF).
MBR Explains: Increasing Access - Key Features of the Affordable Care Act by Year -- 2010
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2010 that sought to increase access to affordable healthcare. As previously mentioned, the Patient Protection and Affordable Care Act was signed by President Obama on March 23, 2010. The law aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key provisions aimed to increase access that took effect in 2010.
MBR Explains: Quality Improvements - Key Features of the Affordable Care Act by Year -- 2010
Continuing our series on the key features of the Affordable Care Act, we will now look into the changes that took effect in 2010 that sought to improve quality and lower cost of healthcare. As previously mentioned, the Patient Protection and Affordable Care Act was signed by President Obama on March 23, 2010. The law aims to increase the quality and affordability of health insurance, lower the uninsured rate, and reduce the costs of healthcare for individuals and the government. However, a number of the mechanisms – mandates, subsidies, and insurance exchanges – are to be rolled out over four years and beyond. Below is an overview of some of the key quality improvement provisions that took effect in 2010.